Case Study
Acute Leukemias of Ambiguous Lineage With FLT3-ITD, Report of 4 Cases
Yi Ding,1 Yi Zhou,2 Ji Yuan,3 Anurag Khanna,4 Linsheng Zhang,4*
1 Department of Laboratory Medicine, Geisinger Health, Danville, PA 17822; 2 Department of Pathology and Laboratory Medicine, University of Miami Miller School of Medicine, Miami, FL 33036; 3 Department of Laboratory Medicine and Pathology, Mayo Clinic, Rochester, MN 55905; 4 Department of Pathology and Laboratory Medicine, Emory University School of Medicine, Atlanta, GA 30322
Abstract
Acute leukemias of ambiguous lineage (ALAL) are a group of acute leukemias either exhibiting no or insufficient markers to define any single lineage differentiation, or expressing antigens of more than one lineage differentiation. The mutation profiles, especially the prevalence, phenotypic features, and additional mutations associated with FLT3-ITD, have not been well studied in ALAL. We report 4 cases of acute leukemias harboring FLT3-ITDs with immunophenotype indeterminate for any single lineage designation. FLT3-ITDs may not be rare in ALAL, including ALAL, not otherwise specified (NOS). Most FLT-ITDs detected in our cases contain insertions at the 5’ end of the ITD sequences. FLT3-ITD appears to be frequently associated with mutations commonly seen in myeloid neoplasms, although not always displaying myeloid lineage-associated antigen expression. Further investigation on the association of FLT3-ITD mutation with the clinical outcome of ALAL, and therapy with tyrosine kinase inhibitors targeting FLT3 are warranted to determine the best options for clinical management for these patients.
Keywords
FLT3-ITD, acute leukemia of ambiguous lineage, mutation profile, immunophenotype.
* Correspondence:
Linsheng Zhang, MD, PhD, Department of Pathology and Laboratory Medicine, Emory University School of Medicine, 531 Asbury Circle, Suite N252A, Atlanta, GA 30322. Phone: 404-712-0582, Fax: 404-778-7944, Email: linsheng.zhang@emory.edu.
Introduction
Acute leukemias of ambiguous lineage (ALAL) are a group of acute leukemias either exhibiting no or insufficient markers specific to any single lineage differentiation, including acute undifferentiated leukemia (AUL), and ALAL, not otherwise specified (NOS), or expressing antigens of more than one lineage differentiation, classified as mixed phenotype acute leukemia (MPAL) [1]. Practically, markers being used to assign a specific lineage differentiation are defined in the World Health Organization (WHO) Classification of Tumors of Hematopoietic and Lymphoid Tissues. Due to the rarity of the AUL and ALAL, NOS cases, our knowledge of the molecular genetic alterations in AUL and ALAL, NOS is limited [2-4]. In the limited number of AUL cases reported, recurrent mutations have been detected more frequently in PHF6, SRSF2, RUNX1, ASXL1 and BCOR genes [5], and double RUNX1 mutations were reported in 3 of 5 AUL cases in one study3. Studies on ALAL, NOS have been included in the ALAL cases, with no specific recurrent genetic abnormalities documented so far.
FMS-like tyrosine kinase 3 (FLT3) belongs to the class III receptor tyrosine kinases (RTKs) that include FLT3, KIT, FMS, and PDGFR (α and β). The signal transduction of FLT3 involves RAS/MAPK, PI3K/AKT and JAK/STAT pathways, related to cell survival and proliferation. Studies on the gene knockout mice targeting FLT3 or FLT3 ligand (FL) revealed that the FLT3 signal pathway is involved in the expansion of hematopoietic stem and progenitor cells of myeloid, lymphoid and dendritic cell lineages [6]. Activating mutations of FLT3 have been found to be one of the most frequent pathological mutations in acute myeloid leukemia (AML) [7], occurring in approximately a third of AML cases, with approximately 23% cases harboring internal tandem duplication (ITD) mutations. The molecular architecture of FLT3-ITD is heterogeneous, with variable lengths and sequences, and integrated at different sites from exon 14 to 15. Recently two subtypes of ITDs have been identified by next generation sequencing (NGS); one type is perfect duplications (typical ITDs) and another contains exogenous or untemplated sequence between the duplicated sequences (atypical ITDs) [8]. In addition, there might be more than one FLT3-ITD variants in any given patient. FLT3-ITD has become a significant prognostic marker of AML, and the molecular features of ITD have been associated with clinical outcomes. Targeted therapy against FLT3 tyrosine kinase, either integrated into the induction therapy or used as monotherapy for relapsed/refractory disease, has been proved to improve the outcome in AML patients with FLT3-ITD [9].
However, FLT3 has not been confirmed to play a specific role in myeloid lineage differentiation. In animal models, constitutive activation of FLT3 contributes to but is not sufficient for the leukemogenesis of acute myeloid leukemia [6]. Although well known for their role in AML, FLT3 mutations are also present in 3-5% of myelodysplastic syndrome (MDS) and approximately 5% of B-lymphoblastic leukemia [10], in which point mutations and indels, not ITDs, of the juxtamembrane domain are more frequently seen [11,12]. FLT3 mutations are also reported in T-lymphoblastic leukemia/lymphoma [13], including early precursor T (ETP) lymphoblastic leukemia/lymphoma [14]. In the limited number of cases studied, FLT3-ITD had a relatively high prevalence in MPAL [15-17], however, it has not been documented in the previously published studies on the mutational profiling of AUL or ALAL, NOS [2-4].
Here we report 4 cases of ALAL harboring FLT3-ITD mutations, with correlation to the immunophenotype and other molecular genetic findings.
Case report
Case 1
A 70-year-old female presented with decreased appetite, fatigue and intermittent nausea for approximately three weeks and had lost 30 pounds of body weight. She had no fever, night sweats, cough, chest pain, dyspnea, abdominal pain, diarrhea, rash, dysuria, or bleeding complications. A routine blood cell count revealed marked leukocytosis with white cell count (WBC) at 337,000/μL with 56% blasts, profound anemia with hemoglobin at 3.4 g/dL, and thrombocytopenia (platelet count 114,000/μL). She was transfused with three units of packed red blood cells and admitted to the hospital. Physical examination found mild splenomegaly but no other palpable masses, adenopathy, or organomegaly. Petechiae were noted on bilateral upper and lower extremities.
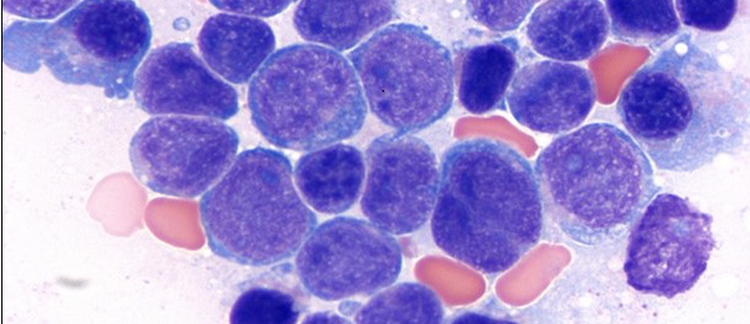
Bone marrow biopsy showed 90% cellularity with blasts comprising 70-80% of the nucleated cells (Figure 1, A and B). The remaining cells are mostly mature lymphocytes and plasma cells, without matured cells to suggest myeloid maturation. By flow cytometric analysis, the blast population expressed partial CD7, CD13, partial dim CD19, partial CD22, CD33, CD34, CD36, variable CD38, partial CD79a (cytoplasmic), partial CD117, CD123, CD200, HLA-DR, and CD45 (dim). Blasts were negative for cytoplasmic CD1a, myeloperoxidase (MPO) and Terminal deoxynucleotidyl Transferase (TdT), CD2, surface and cytoplasmic CD3, CD4, CD5, CD8, CD10, CD11b, CD11c, CD14, CD15, CD16, CD20, CD26, CD56, CD64, and kappa, lambda light chains (Figure 1C). The immunophenotype of blasts, although displaying some myeloid and B-cell lineage differentiation antigens, was not sufficient to assign to any lineage. It was diagnosed as acute leukemia of undetermined lineage, best classified as ALAL, NOS.
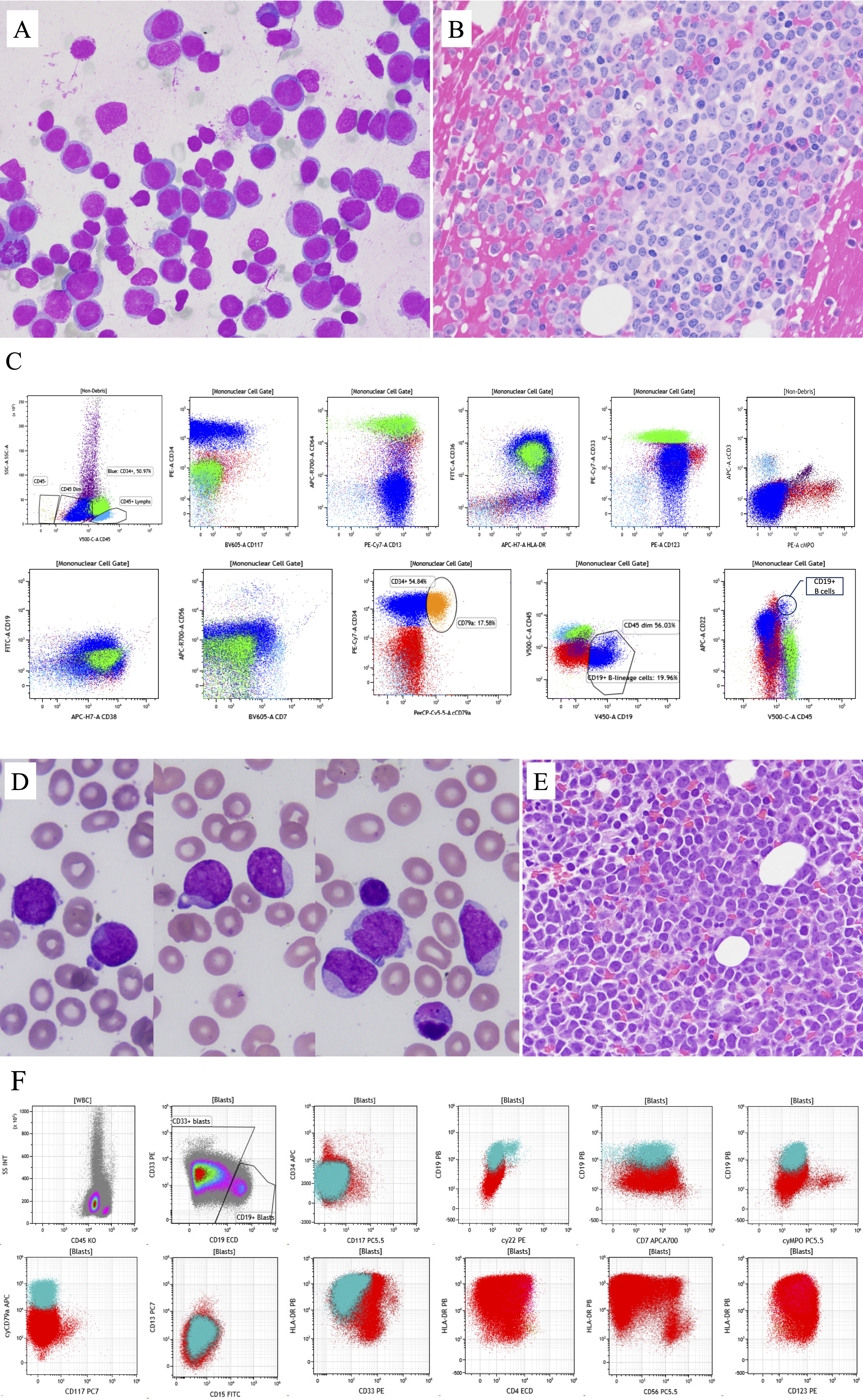
Fluorescence in situ hybridization (FISH) and Q-RT-PCR for BCR::ABL1 fusion were negative. Chromosome analysis demonstrated a normal female karyotype: 46,XX[30]. An amplicon-based, 75 gene/hotspots panel NGS test (VariantPlex MyeloidTM by ArcherDx, Boulder, CO) detected 3 variants of FLT3-ITD (Table 1). In addition, 4 mutations were also detected: RUNX1 [NM_001754.4] c.421T>C (p.S141P) at 90.7%, and 3 mutations in WT1 [NM_024426.4]: c.1110dupT (p.V371fs) at 45.1%; c.1390G>T (p.D464Y) at 9.4%; c.1138delCinsGG (p.R380fs) at 27.4%.
The patient was treated with decitabine + venetoclax and intermittent hydroxyurea. The disease process was complicated by a fall in the bathroom resulting in bilateral subdural hematomas, which resolved about 2 months later. Repeat blood cell counts after 4 months of treatment showed WBC 87.4/μL with 56% blasts. Given the persistent disease, treatment with gilteritinib + venetoclax was started. A bone marrow biopsy 28 days later showed hypocellular marrow with no evidence of acute leukemia. She continued to be treated with gilteritinib with intermittent venetoclax. A lumbar puncture 3 months after starting gilteritinib treatment revealed leukemia involvement in the central nervous system. Intrathecal methotrexate chemotherapy was started, and blasts were negative in cerebral spinal fluid for 4 months. However, a bone marrow biopsy at 7 months after gilteritinib showed relapsed acute leukemia with 70% blast. NGS assay detected low levelFLT3-ITD (66 bp variant, <5%), RUNX1 p.S141P mutation at 75% and an additional new mutation NRAS [NM_002524.4] c.182A>G (p.Q61R) at 42%. The treatment protocol was changed to low-dose cytarabine and intermittent venetoclax. At 15 months after the initial diagnosis, the patient had another fall and acute onset of left-sided weakness. Brain magnetic resonance imaging (MRI) revealed diffuse leptomeningeal disease and cytologic examination of cerebral spinal fluid revealed numerous blasts. The patient was transitioned to comfort care and expired a week later.
Case 2
A 71-year-old female developed headache, bilateral lower extremity swelling, bruising, gum bleeding, and fatigue. A routine blood test revealed a high WBC of 84,000/μL with 82% blasts, thrombocytopenia (platelet count 26,000/μL) and anemia (hemoglobin 8.4 g/dL). On peripheral blood smear, the blasts were variable in size with round to slightly irregular nuclear contour, fine chromatin, conspicuous nucleoli, and scant to moderate amount of cytoplasm. Some blasts had a hand-mirror shape and cytoplasmic vacuole (Figure 1D). Auer rods were not seen. A bone marrow core biopsy showed markedly hypercellular marrow, characterized by sheets of intermediate sized mononuclear cells with fine nuclear chromatin and distinct nucleoli. Background trilineage hematopoiesis was rare. Dysplasia could not be reliably assessed (Figure 1E).
By flow cytometric analysis (Figure 1F), the blasts were moderately positive for CD45 and CD123, variably positive for HLA-DR, CD4, CD7, CD19, CD33, and CD56. Only a small subset of blasts (~15%) expressed strong CD19 and cytoplasmic CD79a without CD10. A separate, very small subset of blasts expressed CD34. Blasts were negative for MPO, cytoplasmic CD3, CD13, CD15, CD64 or CD117. Immunohistochemical stains performed on the core biopsy showed most of the blasts were positive for PAX5 and TdT (variable), while negative for CD3, CD34, CD61, CD117, TCL-1, MPO, muramidase, or E-cadherin.
Cytogenetic analysis identified a normal female karyotype. FISH studies for t(12;21), t(15;17), t(8;21), Inv(16), t(9;22), MLL break-apart, IGH break-apart, del(5q), del(7q), +8, del(20q), or del(17p) were negative. A 54 gene NGS test (NeoTYPE® Myeloid Disorders Profile, NeoGenomics, Fort Myers, FL) identified FLT3-ITD 36 bp (Table 1) and additional mutations, including MLL-partial tandem duplications (MLL-PTD), DNMT3A [NM_022552.4] c.2504C>T (p.T835M) at 48.9%; and CBL [NM_005188.4]c.1243G>A (p.G415S) at 96.3%.
A diagnosis of ALAL was made. She was treated with 7+3 (7 days of standard-dose cytarabine, and 3 days of daunorubicin), followed by allogeneic unrelated donor peripheral blood stem cell transplantation. Unfortunately, the disease relapsed one year after the transplant.
Case 3
A male patient was diagnosed with “AUL” at the age of 11, reportedly hypercellular bone marrow (> 95% cellularity) with sheets of blasts. By flow cytometry, blasts were positive for CD45 (dim-moderate), CD7, partial CD2 (11%), partial dim CD117 (23%), and HLA-DR (14%); negative for cytoplasmic CD3, CD10, CD13, CD19, CD22, CD33, CD34, TDT, MPO. Immunohistochemical stains showed blasts positive for CD99 but negative for CD1a. Molecular genetic testing information at diagnosis was not available. The patient completed treatment with AALL 0434 regimen and achieved hematologic remission without measurable residual disease (MRD) detected by flow cytometric analysis. He continued with daily mercaptopurine plus weekly methotrexate. The recovery process was complicated by immune thrombocytopenia, for which he received Nplate and then splenectomy before normalization of platelet count. He remained in disease remission until age 21 when he was admitted with abdominal/chest pain, cough, low fever, found to have bilateral pulmonary embolisms and circulating blasts.
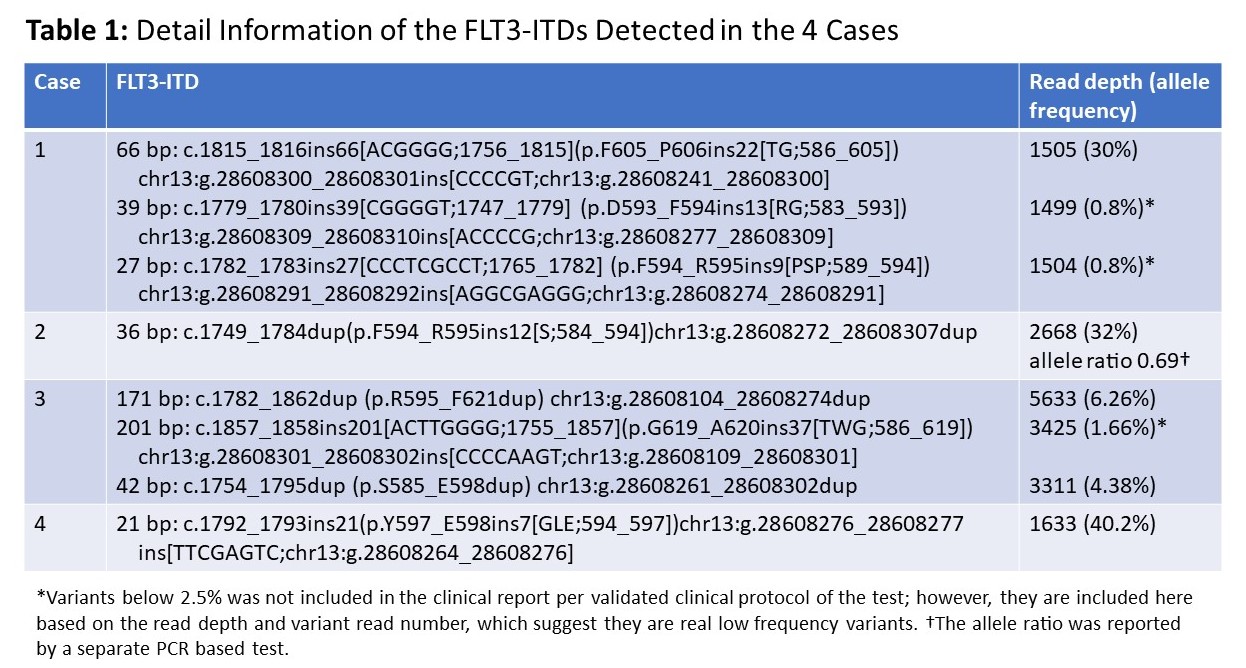
A bone marrow biopsy revealed 95% cellularity with 90% blasts (Figure 2, A and B). Flow cytometric analysis detected a blast cell population comprising approximately 82% of the total events, expressing CD2 (dim), CD7, CD11b, partial CD26, partial CD34, CD38 (dim), CD56, CD123 (dim), CD200 (dim), and CD45 (dim) (Figure 2C). This population was negative for surface and cytoplasmic CD3, CD4, CD8, CD5, CD10, CD11c, CD13, CD14, CD15, CD16, CD19, CD20, CD22, CD27, CD33, CD36, CD64, CD81, CD117, CD138, HLA-DR, cytoplasmic CD79a, MPO and TdT, surface and cytoplasmic light chains. The overall immunophenotypic findings indicate acute leukemia. Given the expression of CD2, CD7, CD56 and lack of myeloid as well as T- or B-lymphoid defining markers in the blast population, NK-lymphoblastic leukemia/lymphoma was considered; however, blasts showed no CD16 expression but displayed CD11b, low-level CD123, and only a small subset expressed CD34, which were unusual compared to NK-lymphoblastic leukemia/lymphoma cases reported in the literature18.
Chromosomes analysis only revealed 1 metaphase with normal karyotype. FISH detected translocation of 11q23 KMT2A in 88% of the cells and gain of one copy of PML (consistent with rearrangement 15q or trisomy 15) in 10% of the cells. No abnormality was detected in chromosomes 5, 7, 8, and no RUNX1::RUNX1T1 or rearrangement involving CBFB was seen. Single nucleotide polymorphism (SNP)-copy number microarray detected gain of whole chromosomes 4, 19 and Y; focal loss of 12p and 17p with breaks within ETV6 and TP53, respectively; focal loss of 14q containing GPHN and focal gain of 6q containing MLLT4, and focal loss of 8p and 9p and loss of Yq. Based on the immunophenotypic and genetic findings, this case was classified as ALAL, likely AUL. NGS panel detected 3 variants of FLT3-ITD (Table 1). In addition, KRAS c.35G>A (p.G12D) was detected in approximately 5% of alleles.
The patient was treated with HyperCVAD (Cyclophosphamide, Vincristine Sulfate, Doxorubicin Hydrochloride and Dexamethasone) followed by AALL 0434 and achieved complete hematologic remission at the last follow up 3 months later, although MRD was detected at 0.082% by flow cytometry.
Case 4
An 83-year-old male with a past medical history of hypertension, and dyslipidemia presented to the Emergency Department with increased fatigue and shortness of breath for two weeks and became confused. He was admitted with leukocytosis (WBC 105,150/μL with 77% blasts), severe thrombocytopenia (platelet count 40,000/μL) and anemia (hemoglobin 8g/dL). Physical examination revealed extensive lymphadenopathy without splenomegaly and pitting edema in bilateral lower extremities. He was treated with apheresis and hydrea.
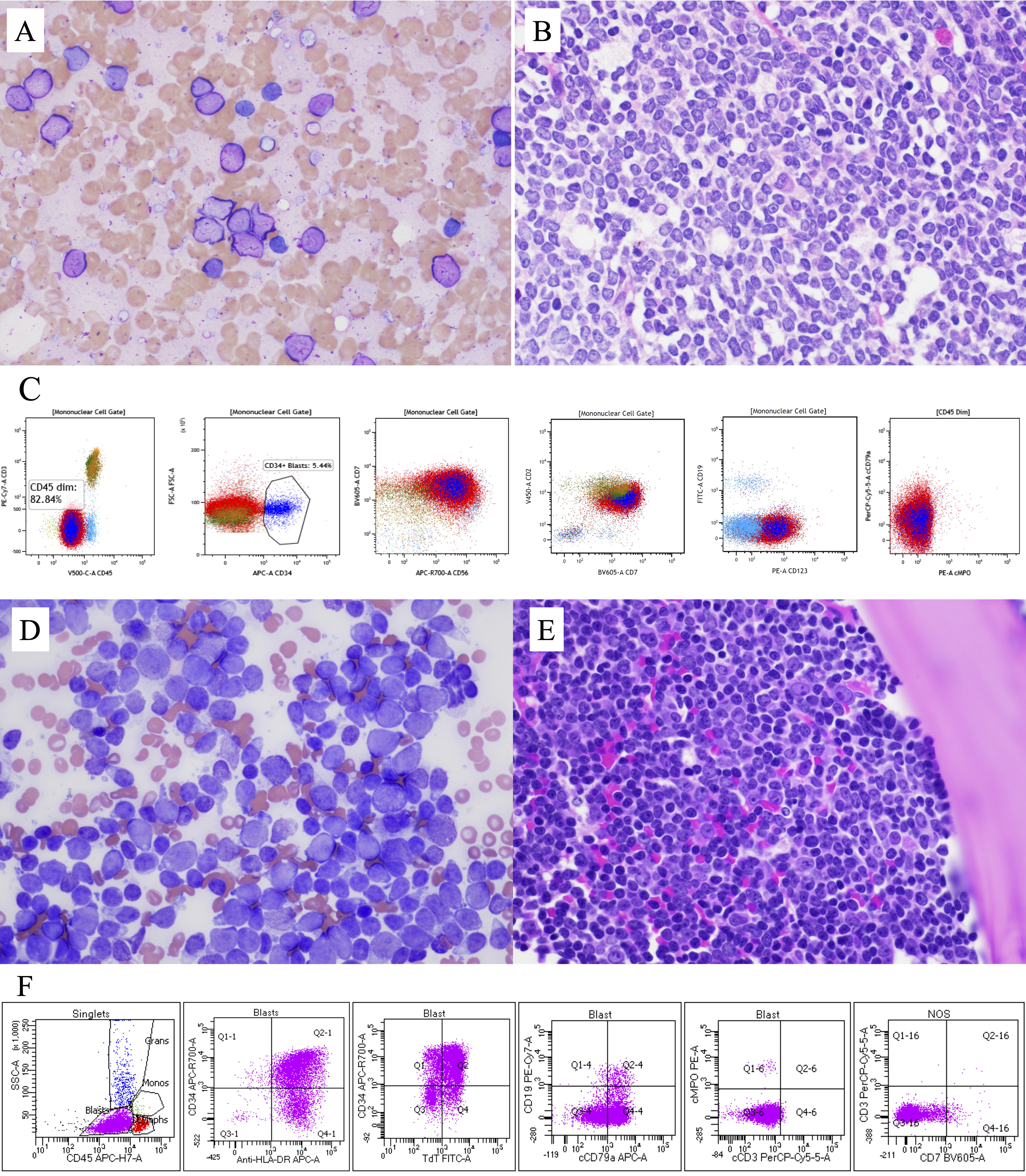
A bone marrow biopsy revealed hypercellular (approaching 100%) marrow with sheets of blasts (Figure 2, D and E). Flow cytometry showed blasts accounting for 88% of total events, with medium to high side scatter (SSC), positive for CD45 (dim), CD13, CD19 (dim, small subset [~10%]), CD34, CD43, CD71 (dim), CD38, HLA-DR, cytoplasmic CD79a (partial, dim), TdT and negative for CD3 (surface and cytoplasmic), CD2, CD4, CD5, CD7, CD8, CD10, CD11b, CD14, CD15, CD16, CD20, cCD22, CD23, CD33, CD56, CD64, CD61, CD117, glycophorin A, FMC7, surface kappa and lambda light chains, cytoplasmic MPO (Figure 2F). The case was considered acute leukemia of undetermined lineage, either an AUL or ALAL, NOS.
Karyotype analysis was unsuccessful due to a lack of metaphase cells. FISH analysis was negative for t(1;19) TCF3(E2A)::PBX1 fusion, t(9;22) BCR::ABL1 fusion, 8q24 (MYC), 11q23 (KMT2A) or 14q32 (IGH) rearrangement or trisomy 4, 6, 10, or 17.
NGS 75 gene myeloid panel detected FLT3-ITD 21 bp (Table 1). Other mutations detected include ASXL1 [NM_015338.5] c.1934dup (p.G646Wfs*12) at 38.8%; EZH2 [NM_004456.4] c.2069G>A (p.R690H) at 47.6%; PHF6 [NM_032335.3] c.5C>A (p.S2*) at 97.9%; SRSF2 [NM_003016.4] c.284C>A (p.P95H) at 51.1%; TET2 [NM_017628.4] c.1209del (p.Q403Hfs*24) at 47% and c.5618T>C (p.I1873T) at 43.2%.
The patient and family decided to pursue hospice without further treatment, and the patient expired within a month.
Discussion
ALAL, NOS is a rare category of ALAL expressing markers not sufficient or specific to be classified as either AUL or MPAL1. The distinction between AUL and ALAL, NOS can be difficult. Expression of T-cell-associated markers, CD5 and/or CD7 without cytoplasmic CD3, and myeloid-associated markers CD13 and/or CD33 without MPO have been documented in ALAL, NOS. The 4 acute leukemia cases reported here are challenging to subclassify. Case 1 showed markers associated with both myeloid and B-lineage differentiation, however, the overall phenotype was not strong enough to be classified as B lymphoblastic leukemia/lymphoma (B-LBL) or MPAL, B/myeloid. Case 2 had a subset of blasts showed markers specific for B-lineage differentiation, combined with PAX5 expression displayed by immunohistochemical stain, this subpopulation met the criteria for B-LBL. However, the large population of blasts showed some myeloid-associated antigens (CD33, CD123), in addition, expressions of CD4, CD56 and CD123 raised the possibility of a blastic plasmacytoid dendritic cell neoplasm (BPDCN). The blasts in this case only expressed low level CD4, partial CD56 and were negative for TCL1. Although not all the markers associated with BPDCN were stained for this case, the phenotype was not entirely compatible with the characteristics of BPDCN. The combined phenotype makes a definite classification very challenging. There is no MPAL, B/ALAL, NOS or MPAL, B/BPDCN defined by the current WHO classification. With the available information, this case is best considered an ALAL, NOS with a subset of blasts displaying features of B lymphoblasts. For case 3, the distinction between NK-lymphoblastic leukemia/lymphoma and AUL is difficult, however, combined all the immunophenotypic features, this case is best classified as AUL [18], although the presence of KMT2A rearrangement has not been documented in any AUL or NK-lymphoblastic leukemia/lymphoma. Case 4 displayed CD13 and partial CD79a expression with a small subset positive for low level CD19, it is therefore borderline between AUL and ALAL, NOS.
FLT3-ITD was reported in 2 of 1417 and 5 of 815 MPAL patients; it was not documented in the 44 AUL or ALAL, NOS cases reported so far [1-5]. In our 4 cases, all FLT3-ITD variants were not the same types of duplications either at DNA or protein (amino acid) level. All 3 variants in case 1, the single short FLT3-ITD variant in case 4 as well as 1 of the 3 variants in case 3 contained exogenous nucleotide and amino acid insertions at the 5’ end of the ITD. Case 2 had a duplication of DNA sequence, however, there was an amino acid change at the integration site. It might be important to recognize these complex insertions because exogenous sequences in ITD have been associated with unfavorable clinical outcome in AML harboring FLT3-ITD [8]. With increased detection sensitivity by NGS, multiple variants of FLT3-ITD in one patient are well documented [19]. Both cases 1 and 3 contained three variants of FLT3-ITD. Based on the variant allele frequencies, the FLT3-ITDs detected in case 3 were only present in subclone(s) of blasts. The clinical significance of multiple variants in one sample, and whether the low-level variants have any significance in the disease course of acute leukemia, need to be further studied. The mutant allelic ratio of FLT3-ITD has been recognized as an important prognostic factor, and a high allelic ratio (>0.5) is associated with a worse prognosis. However, the association between the FLT3-ITD allelic burden and the clinical prognosis was established by PCR-based fragment analysis before NGS tests were widely available in clinical laboratories. Recent studies have shown that hybridization capture-based targeted panel NGS can reliably detectFLT3-ITD and accurately calculate the allelic ratio comparable to that from PCR-based fragment analysis [20]. When the NGS targets are enriched by amplicon-based methods such as the 75-gene panel, there could be skewed amplification of wild type or short duplications; therefore, the allelic ratio needs computational adjustment [21] or to be confirmed by fragment length analysis when clinically indicated, as performed in case 2.
The details of the mutation profiles were not available in the previously published cases of MPAL with FLT3-ITD. Previous studies indicated that FLT3-ITD is not lineage specific [6,10]. Our cases 3 and 4 displayed only minimal markers associated with myeloid differentiation (CD11b in case 3 and CD13 in case 4). However, the additional mutations detected in cases 1, 2 and 4 are frequently associated with myeloid neoplasms. The KMT2A rearrangement detected in case 3 is frequently seen in acute leukemias expressing myeloid and B cell lineage antigens. The additional KRAS mutation is not specific to any lineage either; it has been well documented in both myeloid neoplasms, including AML, and B-LBL. The mutation profiles of our 4 cases suggest that FLT3-ITD may be more likely associated with mutations seen in myeloid neoplasms, despite the lack of definite myeloid phenotype. However, further study on large number of cases is required to confirm this finding. It will also be interesting to investigate the effect of additional mutations on the treatment response and clinical outcome of ALAL cases harboring FLT3-ITD.
The clinical management of ALAL is challenging. In studies comparing different treatment protocols in correlation with clinical outcomes, AUL and ALAL, NOS cases were rare [1]. In our 4 cases, only case 1 received targeted therapy with gilteritinib and achieved a short-term remission despite poor response to decitabine or low dose cytarabine in combination with venetoclax. The follow up NGS result indicated that the FLT3-ITD clone was significantly suppressed and the blasts at relapse harbored a new NRAS mutation. This outcome suggests that targeted therapy against FLT3 tyrosine kinase activity might be a promising treatment option for ALAL patients carrying FLT3-ITD, although a combination with other therapies would be required to obtain a sustainable remission.
In summary, we report 4 cases of ALAL harboring FLT3-ITDs. FLT3-ITDs may not be rare in AUL and ALAL, NOS, and it appears to be frequently associated with mutations more commonly seen in myeloid neoplasms. It is not clear how the mutation profile may affect the immunophenotype of blasts and the clinical outcome of ALAL patients. Further investigation on the therapy with tyrosine kinase inhibitors targeting FLT3 is warranted to determine whether it would be a good option for these patients.
Acknowledgments
The authors claim no conflict of interest.
References
- Aggarwal N, Weinberg OK. Update on Acute Leukemias of Ambiguous Lineage. Clin Lab Med. 2021; 41: 453-466.
- Heesch S, Neumann M, Schwartz S, et al. Acute leukemias of ambiguous lineage in adults: molecular and clinical characterization. Ann Hematol. 2013; 92: 747-58.
- Lao ZT, Ding LW, An O, et al. Mutational and transcriptomic profiling of acute leukemia of ambiguous lineage reveals obscure but clinically important lineage bias. Haematologica. 2019; 104: e200-e203.
- Merati G, Rossi M, Gallì A, et al. Enrichment of Double RUNX1 Mutations in Acute Leukemias of Ambiguous Lineage. Front Oncol. 2021; 11: 726637.
- Weinberg OK, Hasserjian RP, Baraban E, et al. Clinical, immunophenotypic, and genomic findings of acute undifferentiated leukemia and comparison to acute myeloid leukemia with minimal differentiation: a study from the bone marrow pathology group. Mod Pathol. 2019; 32: 1373-1385.
- Small D. FLT3 mutations: biology and treatment. Hematology Am Soc Hematol Educ Program. 2006: 178-184.
- Nakao M, Yokota S, Iwai T, et al. Internal tandem duplication of the flt3 gene found in acute myeloid leukemia. Leukemia. 1996; 10: 1911-1918.
- Schwartz GW, Manning B, Zhou Y, et al. Classes of ITD Predict Outcomes in AML Patients Treated with FLT3 Inhibitors. Clin Cancer Res. 2019; 25: 573-583.
- Daver N, Venugopal S, Ravandi F. FLT3 mutated acute myeloid leukemia: 2021 treatment algorithm. Blood Cancer J. 2021; 11: 104.
- Okabe A, Guirales F, Zhao D, Tirado CA. FLT3 Gene Involvement in B-cell Acute Lymphoblastic Leukemia (B-ALL). J Assoc Genet Technol. 2021; 47: 6-14.
- Elyamany G, Awad M, Alsuhaibani O, et al. FLT3 Internal Tandem Duplication and D835 Mutations in Patients with Acute Lymphoblastic Leukemia and its Clinical Significance. Mediterr J Hematol Infect Dis. 2014; 6: e2014038.
- Zhang Y, Zhang Y, Wang F, et al. The mutational spectrum of FLT3 gene in acute lymphoblastic leukemia is different from acute myeloid leukemia. Cancer Gene Ther. 2020; 27: 81-88.
- Grossmann V, Haferlach C, Weissmann S, et al. The molecular profile of adult T-cell acute lymphoblastic leukemia: mutations in RUNX1 and DNMT3A are associated with poor prognosis in T-ALL. Genes Chromosomes Cancer. 2013; 52: 410-422.
- Neumann M, Coskun E, Fransecky L, et al. FLT3 mutations in early T-cell precursor ALL characterize a stem cell like leukemia and imply the clinical use of tyrosine kinase inhibitors. PLoS One. 2013; 8: e53190.
- Duong VH, Begna KH, Kashanian S, et al. Favorable outcomes of acute leukemias of ambiguous lineage treated with hyperCVAD: a multi-center retrospective study. Ann Hematol. 2020; 99: 2119-2124.
- Noronha EP, Marques LVC, Andrade FG, et al. T-lymphoid/myeloid mixed phenotype acute leukemia and early T-cell precursor lymphoblastic leukemia similarities with NOTCH1 mutation as a good prognostic factor. Cancer Manag Res. 2019; 11: 3933-3943.
- Quesada AE, Hu Z, Routbort MJ, et al. Mixed phenotype acute leukemia contains heterogeneous genetic mutations by next-generation sequencing. Oncotarget. 2018; 9: 8441-8449.
- Weinberg OK, Chisholm KM, Ok CY, et al. Clinical, immunophenotypic and genomic findings of NK lymphoblastic leukemia: a study from the Bone Marrow Pathology Group. Mod Pathol. 2021; 34: 1358-1366.
- Engen C, Hellesoy M, Grob T, et al. FLT3-ITD mutations in acute myeloid leukaemia - molecular characteristics, distribution and numerical variation. Mol Oncol. 2021; 15: 2300-2317.
- He R, Devine DJ, Tu ZJ, et al. Hybridization capture-based next generation sequencing reliably detects FLT3 mutations and classifies FLT3-internal tandem duplication allelic ratio in acute myeloid leukemia: a comparative study to standard fragment analysis. Mod Pathol. 2020; 33: 334-343.
- Tsai HK, Brackett DG, Szeto D, et al. Targeted Informatics for Optimal Detection, Characterization, and Quantification of FLT3 Internal Tandem Duplications Across Multiple Next-Generation Sequencing Platforms. J Mol Diagn. 2020; 22: 1162-1178.