Editorial
Precision Medicine in Hematopathology
X. Frank Zhao
As President Obama mentioned in 2015, “Doctors have always recognized that every patient is unique, and doctors have always tried to tailor their treatments as best as they can to individuals”. “What if matching a cancer cure to our genetic codes was just as easy, just as standard? What if figuring the right dose of medicine was just as simple as taking our temperature?” Therefore, Precision Medicine can be defined as Health care tailored to each individual.
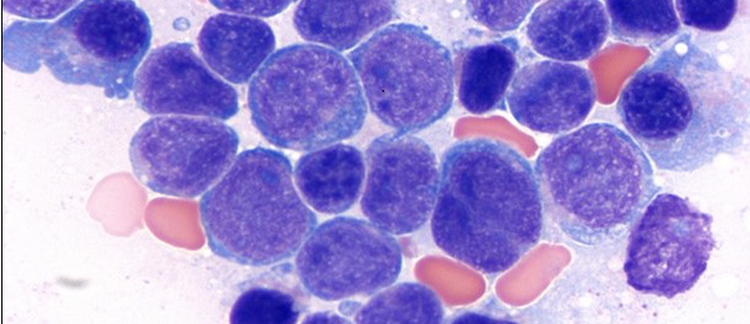
Precision Medicine generally includes two major aspects: 1) specific treatment of diseases based on the defined therapeutic targets; 2) tailored management of patients according to the individual’s genetic and metabolic makeups [1]. Precision Medicine is particularly relevant to Hematopathology for the following reasons: 1) hematological cancers are systemic diseases, often requiring systemic treatment; 2) most of the current standard therapies (Chemo/Radiotherapy) have serious adverse effects; 3) both hematological therapeutic targets and patients’ genetic and metabolic makeups are provided by hematopathologists with the help of molecular pathologists.
The first classical example of targeted therapy is to use Vitamin A to treat acute promyelocytic leukemia [2]. Since then, hematopathologists have been providing the evidence of retinoic acid receptor rearrangements for the clinicians to treat these patients. They routinely provide the evidence of CD20 expression for B-cell lymphomas to be treated with rituximab, a humanized monoclonal antibody [3]. They also routinely provide the ABL1 tyrosine kinase rearrangement for CML which is specifically targeted by the small molecule – imatinib [4]. Nowadays we have hundreds of targeted therapeutic agents that are either already in clinical use or currently still in clinical trials.
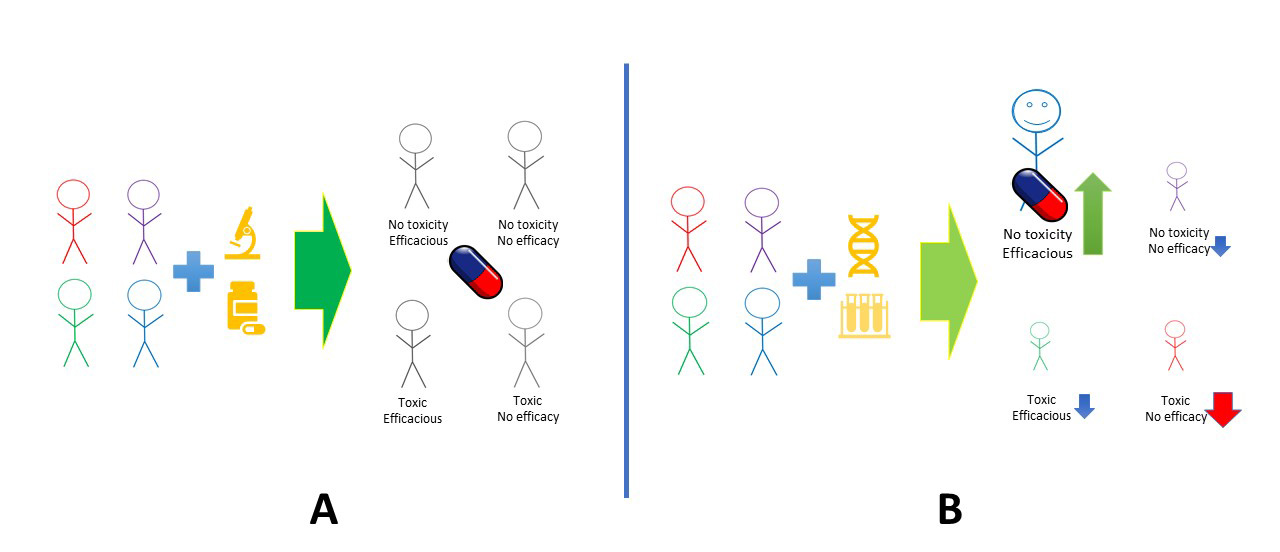
The second aspect of precision medicine is pharcomics, short for pharmacogenomics, pharmacoproteomics and pharmacometabolomics, etc. Hematological malignancies are currently treated based on pathological diagnosis and population-based clinical trials, while ignoring the fact that only a fraction of the patient population that really benefit from the standard therapy (Figure 1A). With pharmacomics-guided precision hematology/oncology, we will be able to treat only the patients who will benefit from the targeted therapy, while avoiding poisoning other patients with the same pathological diagnosis (Figure 1B).
To keep practicing pathologists, hematologists/oncologists, fellows and residents abreast of precision medicine in hematopathology, The University of Arizona College of Medicine Phoenix Department of Pathology invited experts from The University of Chicago, Fox Chase Cancer Center, Philadelphia, Pennsylvania, Emory University and The University of Arizona Phoenix, to share their experiences and perspectives on the practice of Precision Hematopathology. The Pathology Symposium was held virtually on Saturday, February 5th, 2022. One hundred-ninety-four pathologists, cytogeneticists and molecular pathologists had registered for the meeting and this issue will be dedicated to the summary of the presentations.
Reference:
- Zhao XF. Precision pathology: A new frontier. Hematopathology. 2019;3(2):24-25.
- Wang ZY, Chen Z. Acute promyelocytic leukemia: from highly fatal to highly curable. Blood. 2008;111(5):2505-2515.
- Maloney DG, Grillo-López AJ, White CA, et al. IDEC-C2B8 (Rituximab) anti-CD20 monoclonal antibody therapy in patients with relapsed low-grade non-Hodgkin's lymphoma. Blood. 1997;90(6):2188-2195.
- Druker BJ. Translation of the Philadelphia chromosome into therapy for CML. Blood. 2008;112(13):4808-4817.